Did you know that nearly 60 million Americans faced mental health issues from 2021 to 2022? This shows how vital Behavioral Healthcare Revenue Cycle Management (RCM) is. It helps facilities maintain quality patient care as mental health needs grow. The financial side of mental health services is now more important than ever.
A good revenue cycle management system lets healthcare providers focus on patient care. It also monitors billing, coding, and following the rules. Improving these processes can make your facility financially stable and help you continue serving the community well. We'll look into the perks of effective RCM and share tips for excelling in this area.
What Is Behavioral Healthcare Revenue Cycle Management?
Behavioral Healthcare Revenue Cycle Management covers the whole financial process of behavioral health services. It starts with patient registration and ends with collecting payments. This process includes checking insurance, submitting claims, and handling payments.
Billing teams handle these tasks. They ensure all documents are correct and follow rules like CPT and ICD-10 to avoid claim issues.
Behavioral healthcare billing is complex because of the many ways to treat patients. Every step needs careful attention. Good claim management contributes to a smooth revenue flow and helps you focus on patient care.
Challenges Related to Behavioral Healthcare Revenue Cycle Management
Managing the revenue cycle in behavioral healthcare is tough. It involves complex billing for long-term treatments. Changes in insurance coverage make billing hard, leading to billing struggles. Unexpected medical bills can make patients hesitant to get the care they need.
Behavioral services have their own coding rules, making things more complicated. This can lead to claim denials, causing lost revenue and frustration. Over 40% of adults delay medical care because of money worries. This shows how important it is to balance patient care with financial rules.
Why is Behavioral Healthcare Revenue Cycle Management Important
RCM improves financial stability and helps them stand out in a tough market. It also puts patients in more charge of their health. Clear billing builds trust between patients and providers. When patients know their costs, they can make smarter health choices. This leads to more people taking care of their health early and getting the care they need.
With mental health services changing, a solid RCM plan is a must. It helps reduce financial stress and focuses on the patient. This approach keeps patients coming back and improves their experience. Creating a detailed RCM system is good for your organization's money and helps patients stay healthy.
Benefits of Healthcare Revenue Cycle Management
Using a strong healthcare revenue cycle management (RCM) system has many benefits. It helps with billing and makes patients happier, improving your organization's financial health and workflow.
Efficient Billing and Claims Management
A smooth billing process means getting paid on time. It also cuts down on work for your staff, leading to better cash flow and less waiting for money.
Increased Accuracy
Being careful with documents and codes reduces claim rejections. With accurate information, you get paid faster, improving your financial health and meeting your goals.
Better Compliance With Regulations
A good RCM system follows all the rules, lowering legal risks and avoiding fines. It also gives you peace of mind and helps your finances stay strong.
Improved Financial Performance
Improving the revenue cycle leads to better finances. This lets you spend more on patient care and quality. The link between RCM and financial growth is clear. Well-managed RCM leads to growth.
Insightful Data Analysis
RCM systems provide valuable data. This helps you spot trends and improve patient services. Using data leads to better workflow and patient care.
Higher Patient Satisfaction
Good communication during billing builds trust with patients. When patients are happy, they follow their treatment plans better. This helps your organization succeed.

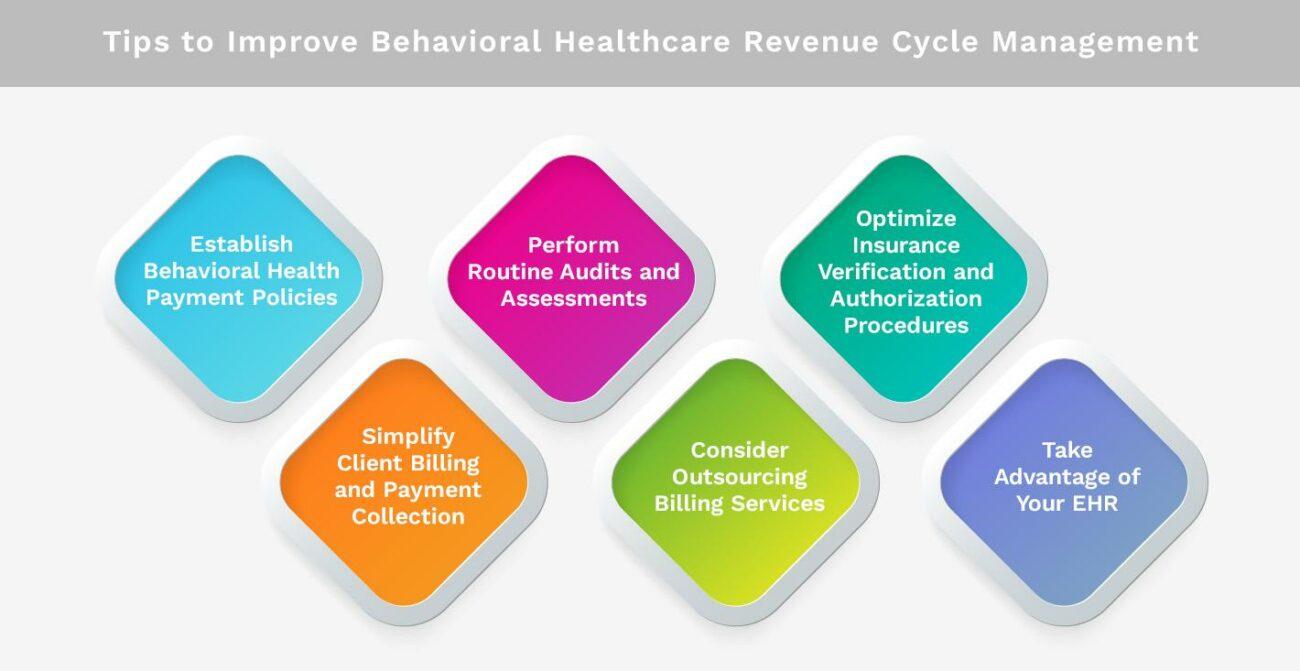
Tips to Improve Behavioral Healthcare Revenue Cycle Management
Improving behavioral healthcare revenue cycle management can make your operations more efficient and profitable. Effective strategies can tackle various challenges, leading to better accuracy in billing and collections. Here are some practical tips to consider.
Establish Behavioral Health Payment Policies
Clear payment policies make it easy for patients to know what they owe. This reduces confusion and leads to quicker payments and fewer disputes. Share these policies through written materials and during the intake process.
Perform Routine Audits and Assessments
Regular audits of billing and coding keep things accurate and efficient. These assessments help spot areas that need work. They can uncover compliance issues and align you with industry standards, making them top billing practices.
Optimize Insurance Verification and Authorization Procedures
Streamlining insurance verification reduces claim denials. Check patient eligibility and
coverage early on. This proactive step can greatly improve your revenue cycle.
Simplify Client Billing and Payment Collection
Online billing platforms make paying easier for patients, improving the experience and improving payment rates. Offering different payment options meets various patient needs, making the process smoother.
Consider Outsourcing Billing Services
Outsourcing billing to experts can free up your staff for patient care. These specialists can improve revenue cycles and ensure you follow the latest rules, leading to fewer mistakes.
Take Advantage of Your EHR
Using Electronic Health Records (EHRs) can improve documentation and reduce errors. EHRs also help streamline billing, which improves financial performance and patient satisfaction.
Why Partner with Kohezion for Behavioral Healthcare Revenue Cycle Management?
Working with Kohezion changes how you handle your revenue cycle in behavioral healthcare. The platform has special software made just for your facility's needs. It makes things more efficient and ties together different parts of patient care.
This includes everything from when patients first come in to when you collect payments. It makes the whole process smooth.
One big Kohezion benefit is getting detailed insights. These insights help you make smart money choices. They make your practice more open and transparent.
This approach makes things run smoother and improves your financial health.
Kohezion also focuses on solving the tough parts of managing patients in behavioral healthcare. Working together can make patients happier and keep your practice strong and up to code. This step is key to improving your RCM strategy and growing your business.
Conclusion
Effective Behavioral Healthcare Revenue Cycle Management is key to keeping mental health services strong and quality high. It helps your organization do better financially and makes patients happier. This approach prevents problems before they start and prioritizes patient care.
Using best practices helps you avoid issues like billing mistakes and follow the rules, leading to a better workflow. Being open and kind in money matters builds trust with patients and the community. Making sure everything is accurate makes things smoother and prepares you for changes in healthcare.
Choosing to improve your revenue cycle is more than just about money. It's about keeping vital mental health services safe and strong. A good RCM sets your practice up for success, which benefits your organization and the people you help.
Contact us today to learn more about how Kohezion can improve your behavioral healthcare revenue cycle management. We can help you implement effective practices that improve financial performance and patient satisfaction.
Start building with a free account
Frequently Asked Questions
To reduce claim denials, ensure that claims are accurately coded and complete before submission. Regularly audit and review claims for common errors and address any issues proactively. Training staff on coding and billing best practices also helps minimize errors and denials.
Technology can help track and analyze revenue data, identify trends, and improve accuracy. Investing in specialized RCM software can increase efficiency and reduce manual errors.
Conduct regular audits of their revenue cycle processes at least quarterly. Frequent audits help identify issues early, ensure regulation compliance, and improve financial performance. Regular reviews also help maintain the accuracy and effectiveness of billing and claims processes.